
One of ZRT's most popular tests includes diurnal assessment of a patient's salivary cortisol levels. On the surface, these tests seem easy enough to interpret, but experienced clinicians know there can sometimes be pitfalls.
Patients testing cortisol in a clinical setting may take undisclosed medications, live under stressful conditions, have inflammation, genetic variations, tumors, and diseases. Sleuthing out the cause of cortisol elevations and depressions can be a real challenge.
To avoid unnecessary work-ups, there are a few areas to consider when interpreting a salivary cortisol test – Contamination, Suppression, and Comorbidities.
Collecting & Processing Samples
The general collection for a diurnal cortisol curve assessment requires drooling into a plastic tube upon waking, another before lunch, again before dinner and a final sample taken before bed.
When the samples arrive at the lab, they're labeled, tested for blood, and centrifuged. Samples are then mechanically pipetted onto separate plates and tested on their own assays. Using an ELISA method, cortisol is quantified using 2 different antibodies and an enzyme marker. In this method, the capture antibody binds to cortisol in the sample with 100% affinity, and the other antibody attached to a special enzyme designed to fluoresce in the spectrophotometer binds to the antibody/cortisol complex and provides the means for quantifying cortisol in the sample.
Contamination
Occasionally, cortisol levels in a sample are grossly elevated beyond what we would expect to see in a Cushing’s patient. Remember that capture antibody with such high affinity to cortisol? It also has a lower affinity to other molecules that have structures very similar to cortisol. If you have direct introduction of hydrocortisone into the saliva sample from the fingers holding the collection tube for example, the high level of substrate overrides that low affinity leading to extremely high reported values that don’t represent endogenous cortisol production at all. Corticosteroid products are so widely available over the counter and many patients don’t even realize they’re using them. So, before reflexing to more diagnostic tests, consider the following case examples demonstrating contamination of the samples.
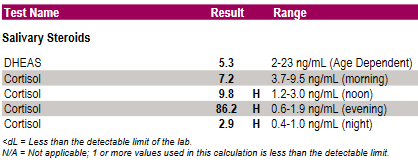
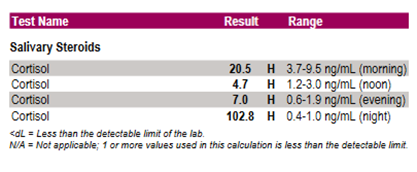
Both of these patients were found to be using a 1% OTC hydrocortisone cream for a rash on the day of collection:
Patient #1:
Patient #2:
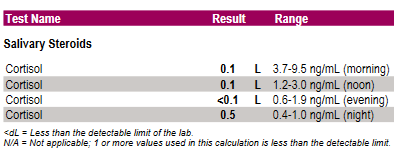
Suppression
Suppression looks very different than contamination in the cortisol results and we see this typically in patients either using daily prednisone therapy or who have had a recent intraarticular steroid injection. So, this may look like an Addison’s case, but it’s really a case of transient adrenal suppression from recent steroid treatment.
If prednisone therapy is discontinued, a period of 4-6 weeks is recommended before testing adrenal function. This is the period of time before the HPA axis is functioning normally again. The same testing window is true for intraarticular steroid injections.
Comorbidities
This one’s obvious, but easy to forget when looking at free cortisol levels in saliva. Some conditions can affect levels of cortisol-binding globulin (CBG) and affect free cortisol levels directly or indirectly. Really understanding the patient’s health status, concurrent medications, and comorbidities will help frame the results for proper interpretation. It may make sense, in addition to saliva testing, to also assess total cortisol levels in serum or capillary blood, or urinary free cortisol levels, for a full 24-hour comparison to aid decision-making. It may also be a good idea to test other aspects of the endocrine system for clues such as thyroid function, sex steroid levels, and insulin, and relate them back to liver and HPA axis function.
Practice Take-Aways
- Remind patients that hydrocortisone can influence their testing even if it is just for that 1 little bug bite.
- When you see extremely high levels > 20 ng/mL – chances are that your patient was using some sort of steroid and does not have Cushing's. Rule that out before worrying about tumors.
- If you have a patient on a steroid therapy and want to check the health of his or her HPA axis, delaying the test for 4-6 weeks after discontinuation is an excellent rule of thumb. For shorter courses, a shorter window may make sense.
Once all of these areas are considered and the pitfalls ruled out, then interpretation of a diurnal cortisol rhythm is a snap! When in doubt, give us a call here at the lab.
