
If you have ever experienced a near-miss collision or other accident, you have likely felt the rush of adrenaline coursing through your veins almost instantly. In that moment, your heart rate, blood pressure, and respiratory rate increased, your pupils dilated, and your brain felt immediately more alert. These are the effects of adrenaline, otherwise known as epinephrine, which is produced in the adrenal medulla when we encounter a significant stressor.
In a “life or death” situation, the stress response can literally save our lives by readying us to act and facilitating a physiological response to support that action. But an extreme stressor isn’t always required to stimulate a stress response. The body is in a constant state of flux and adaptation to our changing internal and external environment, making subtle physiological adjustments to maintain a relatively stable equilibrium known as homeostasis. The maintenance of homeostasis involves the autonomic nervous system (ANS) and the hypothalamic-pituitary-adrenal (HPA) axis through their respective chemical mediators, which include norepinephrine (noradrenaline), epinephrine (adrenaline), and cortisol.
The degree to which these chemical mediators are engaged often depends on the type of stressor and the magnitude of the response. Not all stressors are equal and not all stress is negative. We adapt to the dynamic and challenging situations that we encounter because we are equipped with complex networks that integrate the body and the brain to enhance performance, promote adaptation, and help us to survive (1). If the stress response cannot self-regulate and return to a homeostatic state, disease processes may develop. Testing the levels of these stress mediators can provide useful data that allows for quantifying the effects of stress and implementing strategies to improve both physical and mental health.
A Brief Overview of the Nervous System and the Stress Response
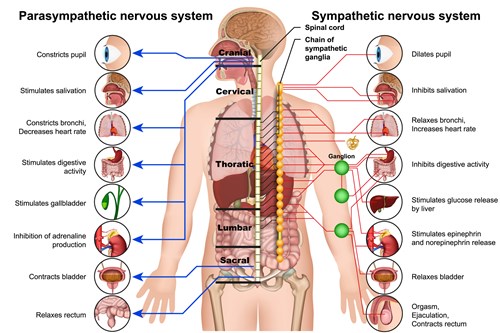
The nervous system is composed of the central nervous system (CNS), housed within the brain and spinal cord, and the peripheral nervous system (PNS), which is further divided into the autonomic and somatic nervous systems. The ANS includes the sympathetic, parasympathetic, and enteric nervous systems (2).
In simple terms, the sympathetic nervous system (SNS) controls the “fight or flight” response, while the parasympathetic nervous system (PSNS) controls the “rest and digest” response. The functions of the sympathetic and parasympathetic branches oppose and complement one another to create balance and maintain homeostasis.
The body’s stress response is mediated by the interplay between the central and sympathetic nervous systems and the HPA axis (3). Upon perceiving a stressor, the CNS relays a signal to the SNS, triggering the release of norepinephrine, which initiates the stress response and primes the body for action. In addition, the SNS signals the adrenal medulla to release epinephrine and additional norepinephrine into general circulation. When epinephrine and norepinephrine bind to adrenergic receptors on target tissues, we experience an increase in heart rate, blood pressure, and cardiac output. The bronchi of the lungs dilate so that we can receive more oxygen to meet the increased demand from the cardiovascular system. Our pupils also dilate reflecting intense concentration and focus. Bodily functions that do not serve immediate survival, such as salivation, lacrimation, urination, and digestion, are decreased (3).
Finally, activation of the stress response stimulates the HPA axis to produce and release cortisol into the bloodstream. Cortisol mobilizes stored glucose, fats, and amino acids to support the energy needed to cope with the stressor. The release of norepinephrine and epinephrine provides an immediate jumpstart to the stress response, while stimulation of the HPA axis and the release of cortisol provides fuel to sustain the response until the stressor is resolved (3).
Norepinephrine, Epinephrine, and Cortisol
Norepinephrine and epinephrine are catecholamines that act as both neurotransmitters and hormones and are vital to the maintenance of homeostasis (4). Catecholamines are synthesized in the brain, in the adrenal medulla, and by sympathetic nerve fibers. About 80% of norepinephrine is produced through the sympathetic nerve fibers with the remaining 20% coming from the adrenal medulla. All the epinephrine produced as part of the stress response comes from the adrenal medulla and is 10 times more potent in its physiological effects than norepinephrine (5).
Norepinephrine functions more as a neurotransmitter as it is primarily a product of the sympathetic nerve fibers and is released directly to receptors on innervated target tissue. Epinephrine functions more like a hormone in that it is released from the adrenal medulla into general circulation where it is transported via the blood to various target tissues (5). Norepinephrine has a stronger influence on blood pressure while epinephrine has a stronger influence on heart rate, contractility, and bronchodilation.
High levels of catecholamines with low cortisol results in a dysregulated stress response. Cortisol secretion, in addition to the activation of catecholamine receptors in target tissues, provides the signal to downregulate the acute stress response. Intense activation of norepinephrine without an adequate rise in cortisol, results in a failure to contain the biological stress response and leads to a persistent stress reaction (6). In the adrenal medulla the enzyme that catalyzes the transformation of norepinephrine to epinephrine is formed only in the presence of high local concentrations of cortisol from the adrenal cortex (7). Low or dysregulated cortisol output can contribute to a recurrent stress loop that cannot resolve appropriately, potentially resulting in elevated norepinephrine. All chemical mediators of the stress response are needed to maintain healthy feedback mechanisms and resolution of the stress response.
Homeostasis and Allostasis
Homeostasis is the ability or tendency of the body to seek and maintain a condition of relative stability as it deals with internal and external changes. The body uses feedback controls and other regulatory mechanisms to maintain a constant internal environment (8). Any physical or psychological event that disrupts homeostasis triggers a stress response. Allostasis is the process by which the body achieves stability or homeostasis through change and reflects the body’s ability to adapt the internal physiological environment to match the external demand (9, 10). A stressful event will stimulate the release of chemical mediators that help us to cope with the situation, while the process of allostasis allows us to return to that homeostatic state.
Allostatic Load
We are always experiencing some form of stress that requires the body to recalibrate to maintain homeostasis. This occurs all day, every day without our awareness. The physiological impact of stress is commonly referred to as the allostatic load. While the chemicals that mediate the stress response have both protective and adaptive effects in the short term, they can result in pathophysiological changes in multiple systems over the long term if produced in deficient or excessive amounts (9).
Allostatic overload occurs when stress is too frequent or longstanding and can result in physiological breakdown (10). The physiological effects of stress brought about by an unmanageable allostatic load can be cumulative over a lifetime and are often the result of modest dysregulation in multiple systems over many years. These cumulative effects are often reflected in basic parameters such as decreased heart rate variability, increased blood pressure, increased fasting glucose, reduced insulin sensitivity, and changes in growth hormone output. Chronically elevated levels of norepinephrine and epinephrine reflect increased sympathoadrenal activation. Under these circumstances, the allostatic load has exceeded the body’s ability to manage the stressor and a return to homeostasis cannot occur (9).
Allostatic Overload, the Stress Response, and Disease
Although the SNS is necessary for basic physiological functions, chronic overactivation can contribute to many disease states. In an article reviewing the maladies and mechanisms of sympathetic overactivity, Fisher et al explore the relationship between sympathetic nerve activation and blood pressure, cardiovascular disease, and metabolic disorders. An overactive SNS has become characteristic of several cardiovascular diseases including ischemic heart disease, chronic heart failure, and hypertension. Outside of the cardiovascular system, excessive activity of the sympathoadrenal system is associated with type II diabetes, obesity, metabolic syndrome, osteoporosis, depression, and an overall acceleration of aging (11).
Stress, Eustress, and Distress
From a psychological perspective, stress can be categorized as good stress or bad stress. Both types of stressors result in the same physiological response. We experience an increased heart rate, breathing rate, and focus, but one sensation is positive and the other is negative. Eustress, or good stress, is a term coined by Hans Selye, MD, PhD, and is often associated with motivation, focus, excitement, enhanced performance, productive energy, and the expectation of a positive outcome. Distress, on the other hand, is associated with procrastination, avoidance, decreased focus, fear, restless energy, impaired performance, and fear of a negative outcome. Some of the main elements that differentiate eustress from distress are the feelings of control within the situation, a predictable timeline, and the ability to handle a situation or task (12). Carter et al further describes distress as emotional stress that involves consciousness, aversiveness, and adrenal stimulation (7).
Particular events and experiences are universally stressful, so to expect that we should never experience distress is unrealistic. Events that trigger the feeling of distress or eustress are often related to our perception, memories, thought processes, past experiences, and genetics. We can modulate physiological stressors through a healthy diet and lifestyle that involves exercise, maintaining a healthy body weight, meditation, reducing factors that contribute to inflammation, and getting adequate sleep. The management of psychological stressors can seem more elusive because multiple factors contribute to how we respond to stressors (see “Anxiety, Depression, and the Cortisol Awakening Response,” July 2021). Whether through a physiological imbalance or a perceived stressful event, the brain and CNS are the starting point of the stress response.
Countering the Effects of Stress by Activating the Parasympathetic Nervous System
To elicit the stress response, we must first have an awareness of the stressor. That awareness occurs in the brain and CNS where we integrate sensorial, physiological, and emotional information and ultimately transmit that information to the ANS (1). Through training and awareness, we can employ methods to activate the PSNS and modify an overactive stress response. If the brain and CNS are where the stress response begins, this is also where we can initiate efforts to subdue or balance the response.
Activation of the PSNS facilitates lowered heart rate, decreased cardiac output, bronchoconstriction, increased sexual arousal, salivation, lacrimation, digestion, defecation, and urination. These are all physiological processes that require a level of relaxation. One method of engaging the PSNS and achieving this balance is through activation of the vagus nerve. The vagus nerve is the 10th cranial nerve and plays an integral role in the activity of the PSNS. It is the longest nerve in the body, originating in the brainstem and extending to the neck, thorax, and abdomen (13).
The vagus nerve contains 80% afferent and 20% efferent nerve fibers, which indicates that most of the communication through the vagus nerve is from the body to the brain. The brainstem is the area of the brain that senses, processes, and regulates most of the autonomic function. The afferent branch of the vagus nerve constantly provides homeostatic parameters from various organ systems to the brainstem, allowing it to respond in a regulatory manner (14).
Vagus nerve activity is modulated by respiration where it is suppressed during inhalation and facilitated during exhalation and slow respiration cycles. Calming activities that involve breath control activate the vagus nerve and promote a sense of relaxation. Various forms of meditation, movement and mindfulness exercises enhance parasympathetic activity primarily through breathing techniques that slow and deepen respiration (14). Other activities that are known to activate the vagus nerve include humming, singing, chanting, cold bathing, sunlight exposure, yoga, pilates, tai chi, social interaction, listening to music, massage therapy, and acupuncture (13).
Positive social interaction and laughter engage and promote the activity of the PSNS. Laughter exercises the diaphragm and forces us to breathe deeply. Being among friends and loved ones can also increase the release of oxytocin, the bonding hormone, which moderates the stress response (15). Daily exposure to sunlight through our eyes and skin reinforces our connection to the cycles of light and dark in which cortisol plays a significant role as a chemical mediator of the circadian rhythm. Regular exposure to sunlight during the day can also promote a better night’s sleep, which is restorative on many different levels (13).
Enhancing vagal tone and engaging the PSNS can improve physical and mental health as well as cognitive function. The physical benefits of increased vagal tone include a decrease in cardiometabolic risk factors and an increase in cardiopulmonary health and fitness, decreased inflammatory markers, and improved general physical function. The mental health benefits include a decrease in perceived stress and an increase in well-being. Cognitive function is enhanced in the area of executive function, working memory, focus, and creativity (14).
Credit: medicalstocks
Assessment of the Stress Response and Related Markers
We can easily rate our perceived stress level through basic questionnaires and lifestyle assessment but to understand the physiological toll of those stressors, we need to measure some basic functional markers. We can assess the physiological effects of our allostatic load by measuring cortisol, epinephrine, norepinephrine, dehydroepiandrosterone sulfate, blood lipid markers and cholesterol ratios, hemoglobin A1c, high-sensitivity C-reactive protein, and fasting insulin, and relate those values to our perceived level of stress. Stress can be difficult to quantify as the experience of stress is unique to the individual; however, we can measure specific markers that reveal the degree to which homeostasis is compromised and this provides us with the opportunity to employ strategies to improve markers that indicate an imbalance.


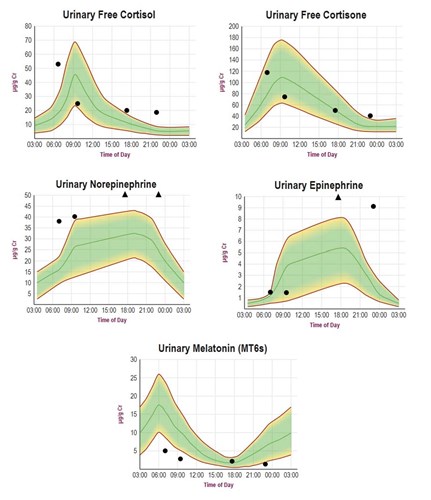
The “NeuroAdvanced Stress Profile” tests urinary levels of five stress markers: cortisol, cortisone, melatonin, norepinephrine, and epinephrine. These markers are tested in dried urine samples by LC-MS/MS from urine collected at four time points (morning, late morning, early evening, and night before bed). Measuring the diurnal patterns of these stress markers provides a much more complete picture of the stress response as opposed to testing only cortisol and cortisone.
In healthy individuals the four data points would be expected to follow close to the center (median) line of each graph within the 20-80% reference range outlined in green. Typical abnormal diurnal patterns of each stress marker are shown for a highly stressed overweight individual with metabolic syndrome. The circadian patterns of cortisol and cortisone are flat, reflecting a poor cortisol awakening response (CAR) and inability of the adrenal glands to keep pace (hypocortisolism) with daily stressors by mid-morning. Diurnal melatonin is flat, which is common with pineal calcification caused by diseases of aging such as metabolic syndrome. The peripheral nervous system neurotransmitters, norepinephrine, and epinephrine are elevated throughout most of the day as a means to compensate for low cortisol to help meet the excessive demands of the stressors caused by metabolic syndrome.
ZRT Test to Consider
- NeuroAdvanced Stress Profile: includes 4x diurnal profiles of urinary Cortisol, Cortisone, Norepinephrine, Epinephrine, and Melatonin measured by LC-MS/MS
References
- Godoy LD, Rossignoli MT, Delfino Pereira P, et al. A comprehensive overview on stress neurobiology: basic concepts and clinical implications. Front Behav Neurosci. 2018;12:127.
- Gershon MD. The Second Brain: A Groundbreaking New Understanding of Nervous Disorders of the Stomach and Intestine. New York, NY. Harper Perennial, 1998.
- Lumen Learning. The Stress Response. Chapter 3: Stress Management. Disease Prevention and Healthy Lifestyles. The Stress Response | Disease Prevention and Healthy Lifestyles (lumenlearning.com). Accessed September 1, 2021.
- Paravati S, Rosani A, Warrington SJ. Physiology, catecholamines. In: StatPearls [Internet]. Treasure Island, FL. StatPearls Publishing, 2021.
- Cryer PE. Physiology and pathophysiology of the human sympathoadrenal neuroendocrine system. New Engl J Med. 1980;303(8):436-444.
- Schelling G, Roozendaal B, De Quervain DJF. Can posttraumatic stress disorder be prevented with glucocorticoids? Ann N Y Acad Sci. 2004;1032:158-166.
- Carter JR, Goldstein DS. Sympathoneural and adrenomedullary responses to mental stress. Compr Physiol. 2015;5(1):119-146.
- Biology Online Dictionary. Homeostasis. https://www.biologyonline.com/dictionary/ homeostasis. Accessed September 1, 2021.
- Karlamangla, Singer BH, McEwen BS, et al. Allostatic load as a predictor of functional decline. MacArthur studies of successful aging. J Clin Epidemiol. 2002;55(7):696-710.
- McEwen BS, Gianaros PJ. Stress- and allostasis-induced brain plasticity. Annu Rev Med. 2011;62:431-445.
- Fisher JP, Young CN, Fadel PJ. Central sympathetic overactivity: maladies and mechanisms. Auton Neurosci. 2009;148(1-2):5-15.
- Shafir H. Eustress vs distress: positive and negative types of stress. Choosing Therapy. https://www.choosingtherapy.com/eustress-vs-distress/. Accessed September 1, 2021.
- Habib N. Activate Your Vagus Nerve: Unleash Your Body’s Natural Ability to Heal. Berkeley, CA. Ulysses Press, 2019.
- Gerritsen RJS, Band GPH. Breath of life: the respiratory vagal stimulation model of contemplative activity. Front Hum Neurosci. 2018:12:397.
- Uvnas-Moberg K, Petersson M. Oxytocin, a mediator of anti-stress, well-being, social interaction, growth and healing. Z Psychosom Med Psychother. 2005;51(1):57-80.
