
When I turned 12, all of a sudden all of my friends were getting their periods, and I just couldn’t wait to get mine! I was so ready to join the ranks of glamorous women who had the privilege of being initiated into the menstruating club. I wanted to belong with them - everything about periods was synonymous with femininity for me at the time. I had to endure witnessing so many of my classmates get the special treatment and be sent home to deal with their cramps, meanwhile staying behind to suffer through boring physics or math classes. Periods seemed to have been happening to everyone around me, just not me. Until one day, seemingly a miracle, I got it! I remember my hands shaking with excitement – I did it – I was in the club! I was becoming a woman! I was beyond thrilled. My 12-year-old dreams were coming true!
My overwhelming excitement lasted for about 10 minutes. What I realized once I got my period was that it wasn’t at all glamorous. It was a messy project in need of careful management. A nuisance really. Once a month for about a week, I had to strategically plan my time around bathroom breaks in between class times in order to deal with the relentless crimson river escaping my body. There was no internet at the time to help me understand what was normal and what wasn’t. I relied on my friends for knowledge about managing cramps and on my parents to let me know just how crabby I’d been during the days leading up to my period.
Is PMDD Worse than PMS? Hint: It Is.
It wasn’t until college that I learned about premenstrual syndrome (PMS), and that it was a real thing. Meaning it happened to many women (not just me) because of specific endocrine fluctuations related to the menstrual cycle. What I also learned in college was that I had the “easy” version – a small percentage of women suffered from something even worse than PMS, called premenstrual dysphoric disorder (PMDD). At the time, this news seemed unfathomable to me – how can you feel even worse? Turns out, you can! And clinical science is just beginning to understand the differences between PMS and PMDD and governing the distressing etiology of the disorder.
What is PMDD?
 PMS symptoms can range from abdominal pain to mood issues, and if they are severe enough to cause functional impairment and interfere with life’s normal activities, they can be classified as PMDD. PMDD is a luteal phase-specific syndrome on the severe end of the PMS spectrum. And it is debilitating! Approximately 3-8% of menstruating women suffer from the same constellation of symptoms as PMS but experienced at a much higher intensity. The burden of PMDD is a cyclical and predictable detriment to the quality of life for the patient and to those around them.
PMS symptoms can range from abdominal pain to mood issues, and if they are severe enough to cause functional impairment and interfere with life’s normal activities, they can be classified as PMDD. PMDD is a luteal phase-specific syndrome on the severe end of the PMS spectrum. And it is debilitating! Approximately 3-8% of menstruating women suffer from the same constellation of symptoms as PMS but experienced at a much higher intensity. The burden of PMDD is a cyclical and predictable detriment to the quality of life for the patient and to those around them.
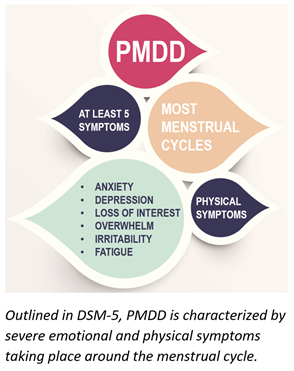
Due to a particular set of cycle-dependent core symptoms, PMDD has recently been outlined as a new diagnostic category in DSM-5 [1]. PMDD is typically defined by having at least 5 symptoms in most menstrual cycles that have to do with severe mood changes and physical symptoms. These symptoms need to occur during the week before and improve shortly after the onset of menses.
How Does PMDD Occur?
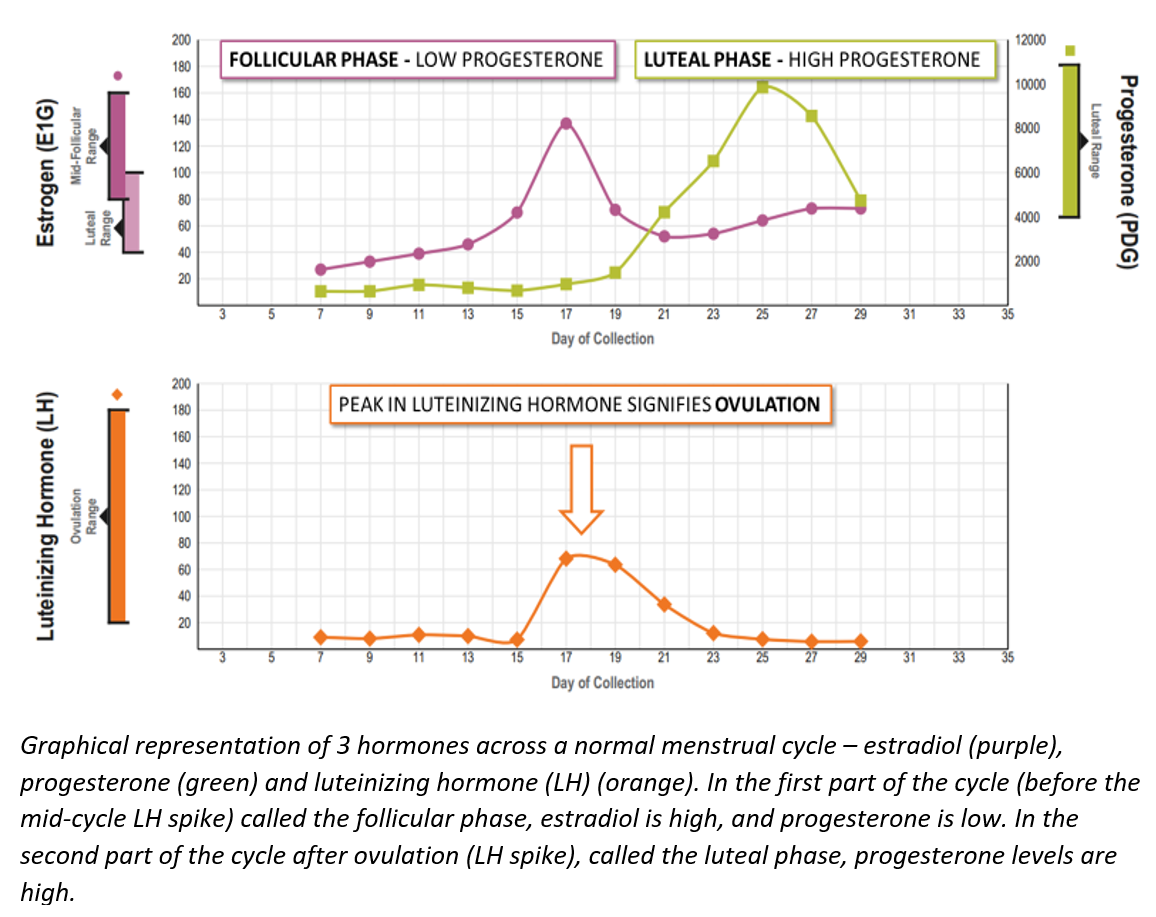 The etiology of PMDD is still largely unclear, but it likely has a lot to do with hormonal shifts across the menstrual cycle. Because PMDD is a luteal phase-specific disorder, it is important to recognize what hormonal changes take place in the luteal phase compared to the follicular phase. One distinguishing feature of the luteal phase is the high levels of progesterone that pick up momentum right after ovulation. This makes sense, as it is the follicle, matured at ovulation, that is responsible for progesterone production to prepare the body for pregnancy, should fertilization take place. Women with PMDD seem to feel relatively well in the follicular phase when progesterone is low, and feel terrible once ovulation occurs and progesterone levels start to rise. So, what exactly could be going on when progesterone – typically regarded as the calming, anxiety-relieving hormone – all of a sudden triggers the opposite reaction in some individuals?
The etiology of PMDD is still largely unclear, but it likely has a lot to do with hormonal shifts across the menstrual cycle. Because PMDD is a luteal phase-specific disorder, it is important to recognize what hormonal changes take place in the luteal phase compared to the follicular phase. One distinguishing feature of the luteal phase is the high levels of progesterone that pick up momentum right after ovulation. This makes sense, as it is the follicle, matured at ovulation, that is responsible for progesterone production to prepare the body for pregnancy, should fertilization take place. Women with PMDD seem to feel relatively well in the follicular phase when progesterone is low, and feel terrible once ovulation occurs and progesterone levels start to rise. So, what exactly could be going on when progesterone – typically regarded as the calming, anxiety-relieving hormone – all of a sudden triggers the opposite reaction in some individuals?
The Answer May Lie with Progesterone Metabolism
The answer may be found in the neuroactive steroid allopregnanolone – a metabolite of progesterone, rather than in progesterone itself. Allopregnanolone levels rise in tandem with progesterone across the luteal phase of the menstrual cycle, and by virtue of targeting the GABA A receptor, produce anxiolytic and sedative effects [2]. In fact, some practitioners recommend progesterone supplementation to manage PMS symptoms. Additionally, IV infusions of allopregnanolone (called Brexanolone) has recently been approved for use in postpartum depression with clinically meaningful improvements in mood [3]. Unfortunately, not everyone responds to allopregnanolone the same way, and in women vulnerable to mood changes in the pre-menstrual period, allopregnanolone can induce negative mood states.
The Inverted U-shaped Effect
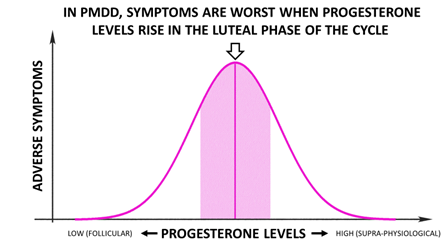 The curious thing about PMDD is that symptomatology can be relieved when ovarian hormones are suppressed altogether, because it is the physiological levels of progesterone-turned-allopregnanolone that are particularly triggering, or when allopregnanolone levels are pushed higher to beyond physiological luteal levels. In other words, at the heart of the disorder are luteal levels of progesterone and allopregnanolone.
The curious thing about PMDD is that symptomatology can be relieved when ovarian hormones are suppressed altogether, because it is the physiological levels of progesterone-turned-allopregnanolone that are particularly triggering, or when allopregnanolone levels are pushed higher to beyond physiological luteal levels. In other words, at the heart of the disorder are luteal levels of progesterone and allopregnanolone.
Although the levels of allopregnanolone between PMDD and non-PMDD groups are not that different [4,5], it turns out that what distinguishes individuals with PMDD from those without is dysregulated GABA A receptor organization. The GABA-A receptor has to mix-and-match the 5 subunits throughout the menstrual cycle in different ways to adapt to the ever-changing hormonal flux [6]. Women with PMDD have previously been reported to exhibit differences in GABA-A subunit structure and abnormal patterns of neural activation [7-9].
The clinical research on PMDD, therefore, points to a role for allopregnanolone in the symptoms of the disorder, with numerous studies finding that allopregnanolone levels typical of the luteal phase (top of an inverted U-shaped curve) trigger adverse symptoms in women with PMDD.
PMDD Therapeutic Management
Management of PMDD requires a careful approach, and unfortunately treatments aiming directly at PMDD are lacking. Instead, focusing on symptom management has been the primary goal of a successful treatment strategy, and clinical research has highlighted a few such approaches. The gist of the therapeutic strategy is to avoid progesterone levels equivalent to normal physiological luteal levels and either bring them down lower or higher than what’s seen in the luteal phase (inverted U-shaped effect). Here are few examples:
- Oral contraceptives – aimed at suppressing ovarian steroids altogether to bring relief for PMDD symptoms [10].
- Selective Serotonin Reuptake Inhibitors (SSRIs) – initiated as soon as symptoms begin and discontinued at menstruation. The short onset of therapeutic action in PMDD could potentially be explained with SSRIs’ ability to enhance formation of allopregnanolone from progesterone by increasing the levels of 5α-reductase in the brain [11], and thus pushing the right side of the U-shaped curve.
- Progesterone – sure, paradoxical and counter-intuitive, but studies show that the maximum concentration of allopregnanolone observed during the luteal phase of the cycle typically worsens the symptoms, yet with a further increase in allopregnanolone with progesterone supplementation, the symptoms decrease in severity [12,13].
- 5α-reductase inhibitors – because allopregnanolone levels observed during the luteal phase of the cycle typically worsens the symptoms, women receiving a 5α-reductase inhibitor to prevent formation of allopregnanolone from progesterone experience a profound reduction in several core PMDD symptoms [4].
The sole comfort of PMDD is that it doesn’t last. It goes away, yet, as sure at it leaves, it comes back the following month. The hope is to make it manageable for patients whose quality of life is compromised with PMDD.
ZRT Laboratory offers a Menstrual Cycle Mapping kit designed to assess cases of PMS and PMDD. Tracking estrogen and progesterone levels throughout the cycle allows us to highlight when the levels are too high or too low, pointing to the root of the problem. Get your Menstrual Cycle Mapping kit today to see if there can be help for your debilitating PMDD symptoms!
Related Resources
- Blog: Feel Awful at "That Time of The Month"? It's More than Just Your Hormones.
- Blog: Hormones, the Menstrual Cycle & Cycle Maps
- Provider Webinar: Mapping the Menstrual Cycle
References
[1] Diagnostic and statistical manual of mental disorders DSM-5, fifth edition ed. 2013: APA, Washington, DC.
[2] Bixo, M., et al., Effects of GABA active steroids in the female brain with a focus on the premenstrual dysphoric disorder. J Neuroendocrinol, 2018. 30(2).
[3] Kanes, S., et al., Brexanolone (SAGE-547 injection) in post-partum depression: a randomised controlled trial. Lancet, 2017. 390(10093): p. 480-489.
[4] Martinez, P.E., et al., 5alpha-Reductase Inhibition Prevents the Luteal Phase Increase in Plasma Allopregnanolone Levels and Mitigates Symptoms in Women with Premenstrual Dysphoric Disorder. Neuropsychopharmacology, 3/2016. 41(4): p. 1093-1102.
[5] Timby, E., et al., Women with premenstrual dysphoric disorder have altered sensitivity to allopregnanolone over the menstrual cycle compared to controls-a pilot study. Psychopharmacology. (Berl. ), 6/2016. 233(11): p. 2109-2117.
[6] Bixo, M., et al., Treatment of premenstrual dysphoric disorder with the GABAA receptor modulating steroid antagonist Sepranolone (UC1010)-A randomized controlled trial. Psychoneuroendocrinology, 6/2017. 80: p. 46-55.
[7] Rapkin, A.J., et al., Neuroimaging evidence of cerebellar involvement in premenstrual dysphoric disorder. Biol. Psychiatry, 2/15/2011. 69(4): p. 374-380.
[8] Berman, S.M., et al., Elevated gray matter volume of the emotional cerebellum in women with premenstrual dysphoric disorder. J Affect. Disord, 4/5/2013. 146(2): p. 266-271.
[9] Gingnell, M., et al., Social stimulation and corticolimbic reactivity in premenstrual dysphoric disorder: a preliminary study. Biol. Mood. Anxiety. Disord, 2014. 4(1): p. 3.
[10] Lopez, L.M., A.A. Kaptein, and F.M. Helmerhorst, Oral contraceptives containing drospirenone for premenstrual syndrome. Cochrane Database Syst Rev, 2012(2): p. CD006586.
[11] Hantsoo, L. and C.N. Epperson, Premenstrual Dysphoric Disorder: Epidemiology and Treatment. Curr. Psychiatry. Rep, 11/2015. 17(11): p. 87.
[12] Andreen, L., et al., Relationship between allopregnanolone and negative mood in postmenopausal women taking sequential hormone replacement therapy with vaginal progesterone. Psychoneuroendocrinology, 2/2005. 30(2): p. 212-224.
[13] Andreen, L., et al., Allopregnanolone concentration and mood--a bimodal association in postmenopausal women treated with oral progesterone. Psychopharmacology (Berl), 2006. 187(2): p. 209-221.
