
Many children with Attention Deficit Hyperactivity Disorder (ADHD) struggle with fitting in and according to some experts, may receive as many as 20,000 negative messages by age 10 than their neurotypical peers. Little wonder then that many struggle with self-esteem and the belief that they are somehow broken. Being labeled as “different” – and this difference perceived as unacceptable to others – can impair an individual’s social development and actually exacerbate their struggles. One study found that children with ADHD whose families expressed high levels of criticism failed to experience the usual decline in symptoms with age, and maintained persistent, high levels of ADHD symptoms into their teenage years. Needless to say, ADHD is often discussed in the context of the problems it presents. It is time for a change that will allow the neurotypical world to make space for neurodiversity with the goal of creating greater well-being for individuals with ADHD and their families.
This blog will provide an overview of ADHD, referencing recent research studies published by experts on ADHD. For a much deeper dive into the etiology of the disorder, please refer to the recently published, World Federation of ADHD International Consensus Statement [1].
How Common is ADHD?
With a prevalence of 5.9%, ADHD is the most common neurodevelopmental disorder in children. Marked by inattention, hyperactivity and impulsivity, the neural mechanisms that underlie these hallmark symptoms vary dramatically from patient to patient, making ADHD a distinct challenge for parents, teachers and health care providers. Stimulant medications, used as first line of treatment, can provide valuable symptom relief for some patients; however, clinical response to specific therapeutic interventions in ADHD is highly individual. Some patients preferentially respond to either methylphenidate or amphetamine preparations, only tolerate non-stimulant therapy options, or achieve symptom remission only on a combination of stimulants and non-stimulants, patterns of which are currently not predictable [2-8]. Some patients can also develop undesirable side effects during the course of treatment (e.g., sleep disturbances, appetite suppression, growth retardation, cardiovascular changes and/or exacerbation of existing tic disorders), which can compromise treatment adherence [1].
Heterogeneity of ADHD
Precisely what makes ADHD so difficult to understand is its heterogeneity, with various genetic and environmental factors likely contributing to the aberrant physiology of the disorder [1]. In other words, the reasons for why someone develops ADHD are as unique as each individual patient [9]. Moreover, to make matters even more complex, besides the classic symptoms described above, many children with ADHD suffer from emotional dysregulation symptoms, such as irritability, aggression, anger issues and negative emotions [10]. Often regarded as distracted, disorganized and disruptive, children with ADHD tend to have difficulty with self-regulation and delayed development of executive functioning skills, leaving many parents feeling lost as to how to create routine and a harmonious family life.
Furthermore, if the disorder persists into adulthood, which in many cases it does, if not well-managed, potential for negative consequences in academic achievement, employment performance and social relationships can present significant detriments to the quality of life for affected individuals.
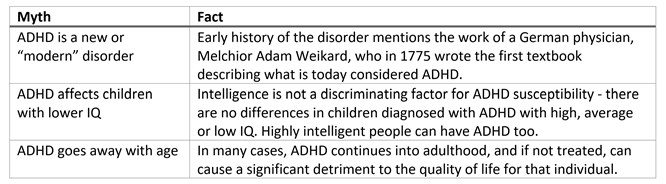
ADHD Myths
There are many myths surrounding the disorder, many of which are dispelled in the World Federation of ADHD International Consensus Statement [1]. Some examples include:

Advantages of ADHD
ADHD can come with its own advantages. Yes, advantages! Of which there are many. The main one is the ability to “think outside the box.” Individuals with ADHD have a natural predisposition to creativity and innovation, refusing to be constrained by conformity. Pushing the boundaries of ordinary concepts in a non-linear fashion, people with ADHD may notice details that others disregard as distractions, and have an intermittent ability to be hyperfocused on their interests, paving the way to conceive cutting edge solutions to existing problems that stumped everyone else.
The Ultimate Goal is to Make Life Easier
The paradoxical nature of ADHD – the swings into super-focused mode during heart-pumping thrills of a quickly changing reality, and the paralyzing overwhelm over the mundane routine – can be very challenging in the day-to-day grind. When a child is easily under- and over-stimulated by the surrounding environment at the same time, parents often seek to ease hyperactivity, improve their child’s focus and balance emotional regulation. In other words, perhaps the ultimate goal in managing ADHD is to do it in such a way that life at home and at school becomes easier and more rewarding for children and their families, while at the same time working with the strengths and positive attributes that ADHD offers.
Diagnosis and Laboratory Testing for ADHD
The diagnostic standard for ADHD takes into account developmental history and symptom evaluation, based on behavior ratings provided by parents and teachers. Although there is no blood test for ADHD at this time, certain laboratory tests can help rule out other conditions that may closely resemble symptoms of ADHD, either mimicking the disorder or exacerbating it. Therefore, there is a real need to augment behavioral diagnostics with supplementary tools supporting a more thorough global clinical assessment.
Vitamin D, not surprisingly, is very important for brain health [11]. Lower maternal vitamin D levels during pregnancy were associated with an elevated risk for the child to develop ADHD [12]. Recent research demonstrates that adding vitamin D as adjunctive therapy to methylphenidate, can reduce ADHD symptoms without adverse effects [13].
The effect of vitamin D supplementation to improve inattentiveness, hyperactivity and behavior was significant but modest, probably because only one nutrient was supplemented. Optimal neurotransmission requires many different types of vitamins and minerals to serve as cofactors in the production of neurotransmitters, and various types of fatty acids to support neuronal membrane structure, with many other micronutrients working overtime in the background. Just keep in mind that even modest effects can all add up eventually to help improve the quality of life for a given individual.
Ferritin - if iron is the readily available merchandise in the front of the store, ferritin is the warehouse in the back. Although no differences have been detected in children with and without ADHD in their iron levels, ferritin levels tend to run low in ADHD [14, 15].
Young bodies undergo tremendous amounts of growth. As the child grows, the body’s stores of iron are stretched to the limit, and unfortunately there is only so much it can absorb from food in one day. Preschoolers and adolescents often have low iron and/or ferritin stores, especially those with ADHD [16]. The last thing that the body will take iron from is blood cells, stealing iron from the liver and brain to make and maintain healthy red blood cells. So, with a low ferritin level, the brain is likely to be starving for this important metal [17].
Why is iron so important you may ask? Well, it is vital for a number of cellular processes including neurotransmitter synthesis (e.g., dopamine and serotonin), myelination of neurons and mitochondrial function [18]. So, does iron supplementation help with improving ADHD symptoms? You bet! After 12 weeks of supplementing ferrous sulfate (80 mg/day), the iron supplementation group showed enhanced attention and reduced hyperactivity and impulsivity [19, 20].
Thyroid hormones play a big role in brain development (hence mental health), even before the child is born. A large Danish cohort study showed that maternal hyperthyroidism during pregnancy (addressed after the birth of the child) was associated with increased risk of ADHD in the child [21]. Indeed, individuals with hyperthyroidism tend to have ADHD-like symptoms, such as anxiety, nervousness, irritability and physical hyperactivity [22].
Specific to thyroid dysfunction and its relationship to ADHD in a pediatric population, research shows that children with a diagnosis of hyperthyroidism have an ADHD prevalence ratio of 1.7 compared to children without hyperthyroidism. This means that if a child is diagnosed with hyperthyroidism, they may or may not simultaneously have ADHD, despite having symptoms that closely resemble ADHD. Without testing for thyroid function, it is impossible to tell whether the symptoms are attributed to innate ADHD or a dysfunctional thyroid system.
Even more notable, in 40% of cases, the mental health diagnosis preceded the diagnosis of hyperthyroidism by 90 days, with ADHD being diagnosed before hyperthyroidism in 68.3% of cases [23]. Let’s stop and think for a moment, because this is a really big deal! Treatments for hyperthyroidism and ADHD are very different. Treating hyperactivity due to hyperthyroidism with stimulant medications will not only not resolve the symptoms, but also may be harmful to the individual.
Nutritional elements like zinc have been reported to be low in urine [24] and in plasma [25] in children with ADHD. Low plasma zinc was reported to have a negative effect on information processing in children with ADHD [25]. Along these lines, some researchers also pay attention to copper levels, specifically presenting evidence that an elevated copper to zinc ratio may significantly contribute to the risk and severity of ADHD [26]. Magnesium was also reported to be low in children with ADHD compared to neurotypical controls [27, 28]. Magnesium deficiency has shown to be linked to fatigue, lack of concentration, nervousness, mood swings and aggression [29]. Some researchers argue that correcting magnesium homeostasis with supplementation may be key to reducing externalizing behaviors [30].
Heavy metals like lead and mercury are potent neurotoxins, meaning that they damage brain tissue, undoubtedly posing a significant threat to healthy brain development [31]. Newborns and young children are particularly vulnerable to the harmful effects of heavy metals with serious long-term ramifications. Even with mild exposure (there is no such thing as a safe level of exposure with heavy metals), children are at risk of developing emotional and behavioral problems, and reductions in IQ that persist into adulthood. Heavy metals typically target the prefrontal cortex area of the brain responsible for (hyper)activity, attention, learning and (anti-)social behavior. Children born to mothers with high mercury exposure during pregnancy, and/or high lead exposure postnatally had higher rates of ADHD, substantiating the fact that these heavy metals are shifting children’s behavior.
Heavy metals contributing to ADHD symptomatology is an example of how genetic, together with environmental factors, can come together to create “the perfect storm” for a neurodevelopmental disorder to establish its roots. A recent study showed that it is children with mutations in genes responsible for neuropsychological function, lead contributed to detriments in the executive function, such as inattention, impulsivity and processing speed [32].
Diet, Sleep & Exercise Considerations
Diet is an important factor in managing ADHD. Dietary approaches to improving ADHD symptoms are beginning to emerge and gain traction in the clinical science community with multi-nutrient intervention studies [33, 34] and clinical trials (clinical trial identifier number NCT03252522).
Besides a multi-nutrient supplement, a diet full of healthy fats, healthy protein and complex carbohydrates may help balance blood sugar and help maintain stable mood and improve focus and concentration. In some instances an elimination diet may help reduce ADHD symptoms, especially if a food allergy is suspected [35]. Additionally, restricting synthetic food coloring may relieve some of the symptoms as well [36]. Small improvements in ADHD symptoms were also reported in studies using omega-3 supplementation [37-39].
Sleep disturbances are reported in upwards of 70% of children with ADHD. Evaluating circadian rhythm abnormalities and correcting them with behavioral interventions and/or melatonin supplementation may be useful in helping achieve the sought-after relief with sleep problems [40]. Reducing screen time throughout the day and especially at bedtime also belongs in this subsection, because the blue light-emitting devices can interfere with melatonin production and likely exacerbate existing problems with sleep.
Lastly, exercise can help improve sympathetic tone and cognitive inhibition in ADHD, improve mood and tire out the little, but very active body. Team and group dynamics can be especially challenging for young people with ADHD, so it’s important to explore the activities they enjoy to find the right fit, often finding a fit in individual sports such as swimming, running, biking and martial arts.
In Conclusion
All the information presented above is intended to enrich the toolkit that health care providers and parents can use to supplement current doctor-recommended approaches to ADHD. Because ADHD is so heterogenous and varies greatly from patient to patient, not one single approach is expected to provide significant symptom relief, but rather to serve as a guide for things to try to see what brings the most symptom relief for a given individual and their family. Even if the improvements in symptoms are small with a specific intervention, the hope is that with a number of slight improvements, the added effect will help ease the burden of the disorder and help foster positive family and peer relationships, successes in the school and work environment, and the positive self-esteem that comes from exploring one’s strengths and interests.
ZRT Laboratory is here to help – samples for many of the tests mentioned above can be collected from finger stick blood collected on filter paper (dried blood spot or DBS). The advantage of collecting blood samples from a finger stick is autonomy for the patient (blood can be collected at home), minimal distress (small blood volumes), which is important in pediatric diagnostics, exceptional sample stability and minimal costs during the shipping of the sample. Talk to your doctor or contact us to help you find a health care provider 1.866.600.1636 info@zrtlab.com to order a test.
Related Resources
- Vitamin D
- Thyroid Imbalance
- Heavy Metals & Nutrients
- Sleep Disturbances
- Serum Testing
- Blog: How Exercise Can Turn the Tide in ADHD
- Blog: Finally Focused: Mineral Imbalances & ADHD (Part 1: Zinc Deficiency & Copper Excess)
- Blog: Finally Focused: Mineral Imbalances & ADHD (Part 2: Magnesium Deficiency)
- Blog: Haunted by Spooky Things in Your Candy?
References
- Faraone SV, Banaschewski T, Coghill D, et al. The World Federation of ADHD International Consensus Statement: 208 Evidence-based Conclusions about the Disorder. Neuroscience & Biobehavioral Reviews. 2021.
- McCarthy S, Neubert A, Man K, et al. Effects of long-term methylphenidate use on growth and blood pressure: results of the German Health Interview and Examination Survey for Children and Adolescents (KiGGS). BMC Psychiatry. 2018;18(1):327.
- Hennissen L, Bakker MJ, Banaschewski T, et al. Cardiovascular effects of stimulant and non-stimulant medication for children and adolescents with ADHD: a systematic review and meta-analysis of trials of methylphenidate, amphetamines and atomoxetine. CNS Drugs. 2017;31(3):199-215.
- Storebø OJ, Ramsstad E, Krogh HB, et al. Methylphenidate for children and adolescents with attention deficit hyperactivity disorder (ADHD). Cochrane Database Syst Rev. 2015;(11): CD009885.
- Schelleman H, Bilker WB, Kimmel SE, et al. Methylphenidate and risk of serious cardiovascular events in adults. Am J Psychiatry. 2012;169(2):178-185.
- Swanson JM, Arnold LE, Molina BSG, et al. Young adult outcomes in the follow-up of the multimodal treatment study of attention-deficit/hyperactivity disorder: symptom persistence, source discrepancy, and height suppression. J Child Psychol Psychiatry. 2017;58(6):663-678.
- Corkum P, Davidson F, Macpherson M. A framework for the assessment and treatment of sleep problems in children with attention-deficit/hyperactivity disorder. Pediatr Clin North Am. 2011;58(3):667-683.
- Hart AB, de Wit H, Palmer AA. Genetic factors modulating the response to stimulant drugs in humans. Curr Top Behav Neurosci. 2012;12:537-577.
- Luo Y, Weibman D, Halperin JM, et al. A review of heterogeneity in attention deficit/hyperactivity disorder (ADHD). Front Hum Neurosci. 2019;13:42.
- Nigg JT, Karalunas SL, Gustafsson HC, et al. Evaluating chronic emotional dysregulation and irritability in relation to ADHD and depression genetic risk in children with ADHD. J Child Psychol Psychiatry. 2020;61(2):205-214.
- Arnold LE. Editorial: A special tree in the forest: from oak to acorn to oak. J Am Acad Child Adolesc Psychiatry. 2021;60(1):26-28.
- Sucksdorff M, Brown AS, Chudal R, et al. Maternal vitamin D levels and the risk of offspring attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2021;60(1)142-151.e2.
- Gan J, Galer P, Ma D , et al. The effect of vitamin D supplementation on attention-deficit/hyperactivity disorder: a systematic review and meta-analysis of randomized controlled trials. J Child Adolesc Psychopharmacol. 2019;29(9):670-687.
- Wang Y, Huang L, Zhang L, et al. Iron status in attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. PLoS One. 2017;12(1):e0169145.
- Tseng PT, Cheng YS, Yen CF, et al. Peripheral iron levels in children with attention-deficit hyperactivity disorder: a systematic review and meta-analysis. Sci Rep. 2018;8(1):788.
- Pivina L, Semenova Y, Dosa MD, et al. Iron deficiency, cognitive functions, and neurobehavioral disorders in children. J Mol Neurosci. 2019;68(1):1-10.
- Cortese S, Azoulay R, Castellanos FX, et al. Brain iron levels in attention-deficit/hyperactivity disorder: a pilot MRI study. World J Biol Psychiatry. 2012;13(3):223-231.
- Hare D, Ayton S, Bush A, et al. A delicate balance: Iron metabolism and diseases of the brain. Front Aging Neurosci. 2013;5(34).
- Konofal E, Lecendreux M, Arnulf I, et al. Iron deficiency in children with attention-deficit/hyperactivity disorder. Arch Pediatr Adolesc Med. 2004;158(12):1113-1115.
- Konofal E, Lecendreux M, Deron J, et al. Effects of iron supplementation on attention deficit hyperactivity disorder in children. Pediatr Neurol. 2008;38(1):20-26.
- Andersen SL, Laurberg P, Wu CS, et al. Attention deficit hyperactivity disorder and autism spectrum disorder in children born to mothers with thyroid dysfunction: a Danish nationwide cohort study. BJOG. 2014;121(11):1365-1374.
- Ahmed OM, El-Bakry AM, Abd El-Tawab SM, et al. Thyroid hormones states and brain development interactions. Int J Dev Neurosci. 2008;26(2):147-209.
- Zader SJ, Williams E, Buryk MA. Mental health conditions and hyperthyroidism. Pediatrics. 2019;144(5):e20182874.
- Arnold LE, Votolato NA, Kleykamp D, et al. Does hair zinc predict amphetamine improvement of ADD/hyperactivity? Int J Neurosci. 1990;50(1-2):103-107.
- Yorbik O, Ozdag MF, Olgun A, et al. Potential effects of zinc on information processing in boys with attention deficit hyperactivity disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32(3):662-667.
- Skalny AV, Mazaletskaya AL, Ajsuvakova OP, et al. Serum zinc, copper, zinc-to-copper ratio, and other essential elements and minerals in children with attention deficit/hyperactivity disorder (ADHD). J Trace Elem Med Biol. 2020;58:126445.
- Effatpanah M, Rezaei M, Effatpanah H, et al. Magnesium status and attention deficit hyperactivity disorder (ADHD): a meta-analysis. Psychiatry Res. 2019;274:228-234.
- Huang YH, Zeng BY, Li DJ, et al. Significantly lower serum and hair magnesium levels in children with attention deficit hyperactivity disorder than controls: a systematic review and meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2019;90:134-141.
- Robberecht H, Verlaet AA, Breynaert A, et al. Magnesium, iron, zinc, copper and selenium status in attention-deficit/hyperactivity disorder (ADHD). Molecules. 2020;25(19):4440.
- Black LJ, Allen KL, Jacoby P, et al. Low dietary intake of magnesium is associated with increased externalising behaviours in adolescents. Public Health Nutr. 2015;18(10):1824-1830.
- Nigg JT. ADHD, lead exposure and prevention: how much lead or how much evidence is needed? Expert Rev Neurother. 2008;8(4):519-521.
- Choi JW, Jung AH, Nam S, et al. Interaction between lead and noradrenergic genotypes affects neurocognitive functions in attention-deficit/hyperactivity disorder: a case control study. BMC Psychiatry. 2020;20(1):407.
- Rucklidge JJ, Eggleston MJF, Johnstone MJ, et al. Vitamin-mineral treatment improves aggression and emotional regulation in children with ADHD: a fully blinded, randomized, placebo-controlled trial. J Child Psychol Psychiatry. 2018: 59(3):232-246.
- Gordon HA, Rucklidge JJ, Blampied NM, et al. Clinically significant symptom reduction in children with attention-deficit/hyperactivity disorder treated with micronutrients: an open-label reversal design study. J Child Adolesc Psychopharmacol. 2015: 25(10):783-798.
- Nigg JT, Holton K. Restriction and elimination diets in ADHD treatment. Child Adolesc Psychiatr Clin N Am. 2014;23(4):937-953.
- Nigg JT, Lewis K, Edinger T, et al. Meta-analysis of attention-deficit/hyperactivity disorder or attention-deficit/hyperactivity disorder symptoms, restriction diet, and synthetic food color additives. J Am Acad Child Adolesc Psychiatry. 2012;51(1):86-97.e8.
- Bloch MH, Qawasmi A. Omega-3 fatty acid supplementation for the treatment of children with attention-deficit/hyperactivity disorder symptomatology: systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2011;50(10):991-1000.
- Chang JP-C, Su KP, Mondelli V, et al. Omega-3 polyunsaturated fatty acids in youths with attention deficit hyperactivity disorder: a systematic review and meta-analysis of clinical trials and biological studies. Neuropsychopharmacology. 2018;43(3):534-545.
- Hawkey E, Nigg JT. Omega-3 fatty acid and ADHD: blood level analysis and meta-analytic extension of supplementation trials. Clin Psychol Rev. 2014;34(6):496-505.
- Esposito S, Laino D, D'Alonzo R, et al. Pediatric sleep disturbances and treatment with melatonin. J Transl Med. 2019;17(1):77.
