
In 2002 several large-scale clinical studies were published on the risks of breast cancer in postmenopausal women using conventional FDA-approved hormone therapy. These were the Women’s Health Initiative (WHI) and Million Women’s studies of women using FDA-approved estrogens and progestogens in the United States and Great Britain, respectively [1,2]. Both studies came to the same conclusion – that estrogen therapy, mostly in the form of oral conjugated equine estrogens, by itself did not significantly increase the risk of breast cancer and, to the surprise of many, was associated with a lower risk. However, when estrogen was combined with a synthetic progestin to prevent uterine cancer, the breast cancer risk increased 1.5 to 2-fold. Virtually all forms, of which there are many, of synthetic progestins increased risk to about the same extent. Smaller studies suggested that FDA-approved oral progesterone, which was not as widely used, did not increase risk in combination with estrogen therapy. These results led to widescale panic among postmenopausal women using conventional estrogen and progestogen (both synthetic progestins and natural progesterone) therapies and a precipitous drop in prescriptions for these forms of HRT [1]. Many women stopped cold turkey all forms of hormone replacement therapy (HRT), which significantly diminished their quality of life. Adverse estrogen deficiency symptoms that were effectively suppressed with estrogen therapy (e.g., hot flashes and night sweats, sleep disturbances, memory issues, incontinence, vaginal dryness, depression, weight gain, etc.) resurfaced with a vengeance in many women, as did risk for diseases of advanced aging (e.g., bone loss and osteoporosis, cardiovascular disease, stroke, diabetes, senile dementia, Alzheimer’s disease). Women were left frightened between “damned if you do and damned if you don’t,” and a large majority chose not to continue HRT. Many health care providers refused to prescribe hormone therapy until more information about risks were made available through clinical trials.
Natural Progesterone Reduces Breast Cancer Risk
When these and other studies emerged in 2002 John Lee, MD, and I along with Virginia Hopkins had just published our book entitled, “What Your Doctor May Not Tell You About Breast Cancer: How Hormone Balance Can Help Save Your Life” [3]. The short of the book is that if your hormones are out of balance and you are suffering from symptoms and conditions of advancing age, meaning the transition into menopause and beyond, then you should replenish your hormones back to physiological levels with the same hormones that your body made when you were healthy early middle age. This meant if you were to use estrogen replacement therapy (ERT) you would replace with estradiol and/or estriol, not a synthetic estrogen like ethinyl estradiol (synthetic estrogen found in birth control pills) or a conjugated horse estrogen (Premarin). And if you were taking a progestogen to help balance the estrogen and protect against its proliferative effects, use bioidentical progesterone, not a synthetic progestin like medroxyprogesterone acetate (Provera) or other synthetic “fake” progesterone. We already knew from earlier studies published several years before WHI that the synthetic progestins were increasing the incidence of breast cancer [3, Chapter 11]. As a research scientist at that time, who had spent 20+ years researching and publishing on the role of estrogen and progestogen binding to their receptors and regulating breast cell proliferation and differentiation, it was clear to me from the research literature and smaller clinical studies that the natural hormone progesterone, when delivered topically at a physiological dose (25 mg) protects normal breast tissue from the growth promoting actions of estrogens [4]. In the breast cancer book [3] we delved into a lot more of what the scientific literature says causes breast cancer and what can be done to help prevent it, like avoid bad foods and environmental chemicals, make sure you’re eating good nutritious foods with plenty of colored vegetables, exercise in moderation, get adequate sleep in the dark, reduce stress as much as possible to lower cortisol-induced estrogen, and take nutritional supplements that bolster the army of antioxidants that protect against environmental toxins that convert good estrogens to bad ones [5,6]. And if your hormones are out of balance, based on testing their levels in body fluids that represent the bioavailable fraction that enters cells, use physiological amounts of bioidentical hormones to adjust them to levels when you were younger and healthy. What has been crystal clear is that bioidentical hormone therapy, if used correctly and in physiological amounts, will significantly reduce risk but is no guarantee you will never develop breast cancer.
Synthetic Progestins Raise Breast Cancer Risk
Fast forward about 20 years to present; several more recent meta-analyses of the risk of breast cancer with FDA-approved, or equivalent for non-US countries, estrogen and progestogen therapies, shed some new light on risk of HRT for breast cancer. These studies (US, British) mostly just reiterated what we already knew: that estrogen therapy only increases breast cancer risk slightly, but significantly when combined with synthetic progestins [1]. The meta-analysis of prospective studies of slightly over 100,000 women using estrogen alone or estrogen combined with progestogens (mostly synthetic), but also oral progesterone [1], revealed that estrogen therapy alone was only associated with a slight increase in risk, but when combined with a synthetic progestin the risk was approximately doubled after 5 years and doubled again at 10 years of use. No question, synthetic progestins were bad for the breasts and should not be used, especially by women who want to reap the many benefits of hormone therapies their entire lives, who should avoid synthetic progestins. Most surprising was that this study also reported that FDA-approved oral bioidentical progesterone, combined with estrogen, carried the same approximately 2-fold higher risk at 5-10 years, but strangely had no increased risk less or greater than that [1]. No data were available for topical progesterone combined with estrogens, perhaps because very few, if any, clinical studies have been carried out in the US or Great Britain and surrounding European countries using natural progesterone delivered topically.
Topical versus Oral Progesterone
Despite research and small clinical studies showing that natural progesterone delivered topically directly to the breasts of humans [4] and primates protects against estrogen-stimulated cell proliferation of normal mammary epithelial cells, a risk factor for breast cancer, surprisingly no large prospective randomized clinical studies have been carried out to investigate if topical progesterone therapy is associated with reduced risk for developing breast cancer. The reason for this is not based on science, but economics. Progesterone cannot be patented; however, progesterone combined with a special delivery system can be, as seen with several forms of FDA-approved oral progesterone (Prometrium and Bijuva). Oral progesterone, however, while it protects the endometrial lining, may not raise progesterone to a level high enough to counter the growth-promoting actions of estrogens in the breast tissue [7].
Factors Influencing Estrogen Metabolism to Mitigate Risk
What is clear is that anything that reduces excessive estrogen burden, be it progesterone, natural or synthetic aromatase inhibitors, diet with more fiber and phytochemicals with colored vegetables, exercise, stress reduction, better sleep habits, etc., translates to lower breast cancer risk. That is what progesterone does. It lowers cell proliferation by down-regulating estrogen receptors (ER), preventing further estrogen-mediated stimulation of cell proliferation and redirects differentiation through progesterone interaction with estrogen-regulated cellular progesterone receptors (PR). Progesterone, via its activation of 17β-hydroxysteroid dehydrogenase type 2 (see diagram below), also increases the conversion of estradiol, a potent estrogen with high affinity for cellular ERs, to estrone, a weak inert estrogen [3]. Progesterone also enhances synthesis of sulfotransferase, an enzyme that then sulfates estrone to estrone sulfate, which is unable to enter cells and serves as a circulating estrogen precursor that must be converted back through two enzymatic steps, sulfatase and 17β-hydroxysteroid dehydrogenase type 1, to estradiol.
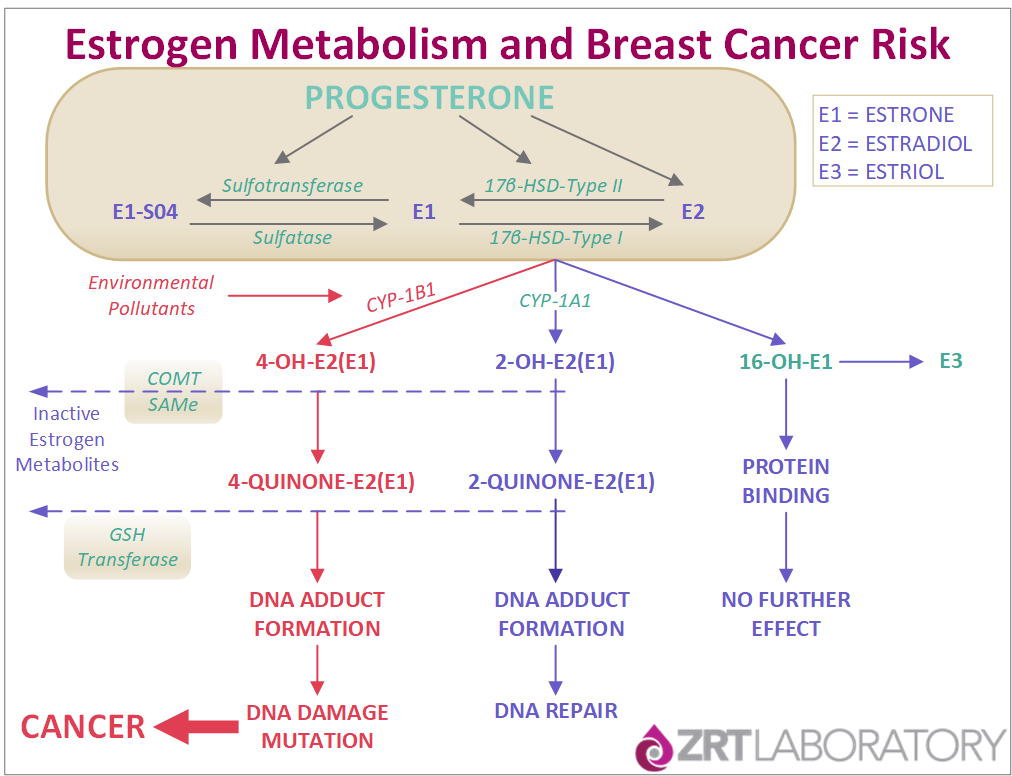
Diagram depicts the progesterone-regulated metabolism of E2 to E1 and then to E1-SO4, and then Cyp1A1 and Cyp1B1 conversion, respectively, to 2- and 4-hydroxy estrogens and their further oxidation to 2- and 4-quinones. For details see reference [5].
Progesterone’s Effects on Estrogen-Stimulated Cell Proliferation
What is poorly understood in the scientific/clinical community is that progesterone has dual actions in its effects on estrogen-stimulated cell proliferation. At the lower luteal levels (about 1-10 ng/mL) progesterone synergizes with estrogen to promote cell proliferation with little differentiation. If insufficient progesterone is produced in the presence of high estradiol, as often occurs at perimenopause with compromised luteal function, proliferation may be higher than with estradiol alone [7]. However, at higher luteal levels (10-30 ng/mL) progesterone counters the growth-promoting actions of estrogen by down-regulating ER, and through induction of cellular PR redirects the cellular machinery to drive quiescence and differentiation, causing proliferation to come to a halt. If inadequate progesterone is present, as often happens at the transition to menopause (perimenopause) when the corpus luteum fails to produce adequate progesterone but abundant estrogen (low progesterone/estradiol ratio), then the combination of higher physiological estrogen and lower luteal progesterone (in range, but low-normal) will often result in persistent proliferation and the clinical manifestation of fibrocystic and painful breasts. Excessive proliferation in the absence of progesterone increases risk for gene mutations that have the potential to lead to increased breast cancer risk.
Risks Greatest During the Menopausal Transition
As shown in the diagram above, estrogens in excess, in the absence of progesterone and with exposure to environmental toxins, induce the cytochrome enzyme Cyp1B1 that converts beneficial estradiol to potentially toxic and mutagenic 4-catechol estradiol [5,6]. During this perimenopausal transition is when the rate of increase of breast cancer is greatest. Retrospective clinical studies have shown that the higher the luteal progesterone level 5 years prior to breast cancer diagnosis, the lower the risk of developing breast cancer [8], so it is important to keep progesterone balanced with estradiol, especially during the menopause transition when estrogen metabolite damage is most likely to occur, as shown in a recent study on estrogen metabolite formation and breast cancer risk [6].
Topical Progesterone Achieves Optimal Tissue Levels
As mentioned, oral progesterone, because it is mostly degraded (90-95%) in the GI tract and liver to metabolites with no capacity to bind and activate PR, may not reach sustained luteal levels to counter the growth-promoting actions of estrogens. Based on saliva, capillary blood, and tissue levels of progesterone, only topically applied progesterone [9] can achieve capillary blood and tissue levels of progesterone high enough to counter the proliferative actions of estrogens. While small clinical studies have shown that topical progesterone used at physiological dosing (25-50 mg) effectively reduces estrogen-induced proliferation of the mammary epithelium in humans [4], this form of therapy has not been tested in a large scale prospective case-control randomized study as with FDA-approved conjugated equine estrogens in combination with synthetic progestins [1,2].
What might we learn from what we know about the dual actions of progesterone as it relates to bioidentical estrogen and progesterone therapies for menopausal women and their risk for breast cancer? If we let mother nature be our guide, then we should strive to keep estrogen within the physiological ranges seen throughout a full monthly cycle (about 50-150 pg/mL in serum or about 2% of that seen in saliva, 1-3 pg/mL). For at least half of the month serum or capillary blood (Dried Blood Spot, DBS) progesterone should be about 10-30 ng/mL and saliva 200-600 pg/mL. This results in a progesterone/estradiol ratio of about 100-300, which is consistent with the ratio seen at the peak of the luteal phase and shown to be protective of the breasts exposed to estradiol [4]. Excessive estradiol or too little progesterone will result eventually in estrogen dominance and symptoms of estrogen excess (e.g., weight gain in the hips and thighs, fibrocystic and painful breasts, mood swings, etc.) Those are warning signs. High levels of 4-catechol estrogens ratchet that up to extreme warning [5] as we have found that 4-catechol estrogens are much higher in women harboring breast cancers than healthy women [6].
Many providers believe that topical progesterone is ineffective because it doesn’t raise serum levels. To the contrary, we [9] and others [4,10] have shown that physiological dosing with topically delivered progesterone raises the progesterone to physiological levels in tissues of the body such as the salivary gland, and capillary beds of the finger tips. High dose progesterone (> 50 mg), in an attempt to achieve physiological concentrations in serum never does this, regardless of the topical progesterone dose [9]. What may seem paradoxical based on serum levels is that excessive progesterone and too little estrogen will eventually keep ER persistently down-regulated and may precipitate symptoms of estrogen deficiency with weight gain, vasomotor symptoms, excessive sleepiness, etc. Keep in mind that estradiol and progesterone are produced in a rhythmic pattern each month. Estradiol rises slowly throughout the first half of the cycle and peaks about midway with ovulation. This stimulates growth and proliferation of the uterus and breasts. Progesterone will not work if there is no cellular PR, which requires adequate ER. Excessive progesterone down-regulates ER, stopping the cycle.
In summary, maintaining estradiol levels in balance with natural progesterone is necessary to achieve optimal clinical benefits of these hormones. It is the opinion of this author that these goals for optimal progesterone therapy as a breast cancer preventive can best be achieved with topical progesterone, and not oral progesterone, or a synthetic progestin. However, clinical studies with topical progesterone are needed to confirm this hypothesis.
While you go through the stages of menopause, it is important to get your hormone levels checked to ensure that you are within physiological levels. If you are going into, in the middle of, or at the end of your menopause journey, ZRT's saliva and blood spot testing can give you the information necessary to get your hormones balanced and get you back to optimal health.
This article was first published in the American Academy of Anti-Aging Medicine (A4M) Winter 2019 Issue.
Related Resources
- Blog: Genetic Sequence Variations and Breast Cancer Risk
- Blog: Topical Delivery of Sex Steroid Hormones and Distribution in Different Body Fluids
- Blog: New Research Shows Natural Progesterone Can Help Treat Breast Cancer Part 1 and Part 2
References
[1] Collaborative Group on Hormonal Factors in Breast Cancer. Type and timing of menopausal hormone therapy and breast cancer risk: individual participant meta-analysis of the worldwide epidemiological evidence. Lancet. 2019;394:1159-68.
[2] Manson JE, WHI Investigators, et al. Menopausal Estrogen-Alone Therapy and Health Outcomes in Women With and Without Bilateral Oophorectomy: A Randomized Trial. Ann Intern Med. 2019;171:406-414.
[3] Lee JR, Zava D, Hopkins V. What your doctor may not tell you about breast cancer – how hormone balance can help save your life. Warner Books, 2002.
[4] Chang KJ, et al. Influences of percutaneous administration of estradiol and progesterone on human breast epithelial cell cycle in vivo. Fertil Steril. 1995;63:785-91.
[5] Cavalieri EL, et al. Molecular origin of cancer: catechol estrogen-3,4-quinones as endogenous tumor initiators. Proc Natl Acad Sci USA. 1997;94:10937-42.
[6] Miao S, et al. 4-Hydroxy estrogen metabolite, causing genomic instability by attenuating the function of spindle-assembly checkpoint, can serve as a biomarker for breast cancer. Am J Transl Res. 2019;11:4992-5007.
[7] Sitruk-Ware LR, et al. Inadequate corpus luteum function in women with benign breast diseases. J Clin Endocrinol Metab. 1977;44:771-4.
[8] Micheli A, et al. Endogenous sex hormones and subsequent breast cancer in premenopausal women. Int J Cancer. 2004;112:312-8.
[9] Du JY et.al. Percutaneous progesterone delivery via cream or gel application in postmenopausal women: a randomized cross-over study of progesterone levels in serum, whole blood, saliva, and capillary blood. Menopause 2013;20:1169-75.
[10] Leonetti HB, et al. Topical progesterone cream has an antiproliferative effect on estrogen-stimulated endometrium. Fertil Steril. 2003;79:221-2.
