
For the past 4 weeks, each morning for me starts with a cup of coffee and a side of news about the global health pandemic in which we’re living. Invading our world rapidly, forcing everything to look different today compared to just a month ago, COVID-19 has everyone on high alert! Throughout the rest of my day, I allow myself to be interrupted by articles about the virus, nurturing the feelings of surrealism and unease. Quarantined together with my family, my new reality has been reduced to a filtrate of information through the COVID-19 prism. It’s disorienting how quickly the normalcy of our regular lives have been swept away with the state-mandated stay at home orders. This is starting to feel like the opening scenes of a post-apocalyptic film, rather than reality. As a scientist, I grapple with uncertainty – there are so many questions about what is happening right now, with only few answers, as we’re all witnessing this epidemic unfold. So below is a list of things that I found helpful in understanding the widespread COVID-19 infection, the immune response, and the reasons behind social and physical distancing.
SARS‐CoV‐2 = type of coronavirus.
COVID-19 = COrona VIrus Disease – the name for the actual infection or disease caused by SARS‐CoV‐2.
Naming Semantics
Many things can be confusing during a health crisis, so let’s start with the language we use when talking about the current state of affairs. Coronaviruses (also known as CoV in medical jargon) belong to the same family of viruses as Severe Acute Respiratory Syndrome (SARS) and Middle East respiratory syndrome (MERS), but usually cause only mild illnesses (e.g., common cold). On February 11th 2020 the coronavirus study group of the International Committee on Taxonomy of Viruses named the novel coronavirus as severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2); and the World Health Organization (WHO) formally named the disease triggered by SARS‐CoV‐2 as coronavirus disease 2019 (COVID‐19).
Crown-Like
Coronaviruses are called “corona” because of the crown-like projections that protrude from their surface – on the outside the virus structure is enveloped in a casing of lipid molecules with protein spikes [3]. This oily lipid structure falls apart on contact with soap; this is why washing your hands is important to prevent or at least minimize the spread of illness.
How does it Work?
For a great explanation on how viruses enter and hijack cells inside a human body, the following illustrations from the New York Times are helpful. In a nutshell, SARS‐CoV‐2 is transmitted from human to human, via respiratory droplets or close contact [4]. It freely enters the body through the airway, the spike proteins of the “crown” associating with the angiotensin-converting enzyme 2 (ACE2) surface receptors on alveolar (lung) cells, and the virus is ushered inside (Fig. 1) [5]. Once inside the cells, the virus releases its genetic material (RNA) and hijacks the human cell machinery to make viral proteins. So, in a sense, the virus overrides the cell’s normal programming and forces it to become a virus-making factory.
How Does It Feel?
As the infection continues to progress, fever and cough might develop – a sign that the immune system is fighting back. If the infection continues, it can damage alveolar cells and further stimulate a systemic inflammatory reaction. If this happens, it becomes harder for the lungs to supply oxygen for the blood to carry to various organs. Instead, lungs can fill up with fluid, making it hard to breathe. If the infection is severe enough, some may even need a ventilator.
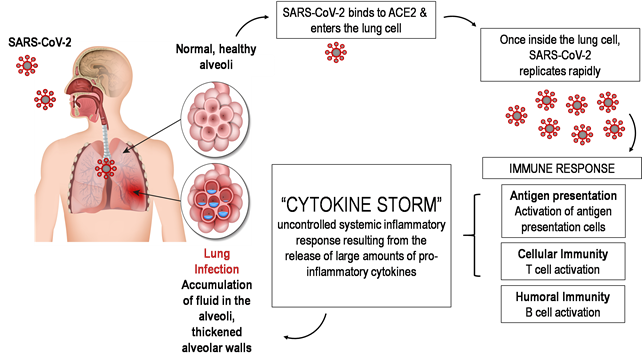
Fig. 1 Proposed model for the host immune response to SARS-CoV-2 infection. Adapted from [1] & [2].
The infection process and the immune defense are extremely complicated [3]. A case report for a moderate COVID-19 infection highlights the complexity of the immune response dynamics in a 47-year-old female patient [6]. Based on a good number of recent reports and the CDC, common symptoms of COVID-19 are [7]:
- 98% of the patients in the study had fevers
- 78% had a temperature higher than 38°C (100.4 oF)
- 76% of the patients had coughs
- 44% of patients experienced fatigue and muscle pain
- 55% of patients had difficulty breathing
- 28% developed phlegmy coughs
- 8% had headaches
- 3% had diarrhea
- 100% of patients showed abnormalities in chest computed tomography - grinding glass‐like and consolidation areas were found in 98% of the infected patients' lungs bilaterally
Why Social Distancing?
Just a short while ago, the terms “flatten the curve” and “social distancing” didn’t mean much to any of us. Today, on the other hand, that’s all we hear on the news and through social media. So why exactly do we bother with all this self-isolation business; why not just have a COVID party, be sick all at once, and get over it all at once? Ok, let’s break this down, using stats from the Chinese Center for Disease Control and Prevention [8]:
- By rough approximation there are 350,000,000 people in the US, and we all have a “COVID PARTY” → all get infected all at once
- 80% of us are going to be “just fine” with mild pneumonia or nothing at all → no big deal
- 14% or 49,000,000 of us are going to develop severe disease (difficulty breathing, not enough oxygen) → not great
- 5% or 17,500,000 will develop critical disease with respiratory failure, shock and multiorgan dysfunction. So that’s roughly 350,000 people per state → that’s a problem. According to OPB, Oregon has only 6,601 staffed hospital beds. So…
- And that’s precisely why we don’t want to get infected all at once
There’s No Treatment (Yet) - But Here’s What You Need to Know
The burst of confirmed cases worldwide shows how detrimental SARS‐CoV‐2 can be to human health. With no preventative vaccine and no curative treatment for COVID-19, relying on our own immune system to protect us from the threat of COVID is one of our best options for now. Just to be clear, there's no magic food or pill that is guaranteed to boost your immune system and protect you against the virus. However, there are ways to keep your immune system functioning optimally, which can help to keep you healthy and give you a sense of control in an uncertain time.
Estradiol is a female sex steroid and its actions extend way beyond reproduction – it plays an important role in modulating immune events as well [9, 10]. It seems appropriate to talk about sex steroids in the context of SARS-CoV-2 as it appears that men and women are equally likely to contract the virus, but men have a harder time fighting off the infection. Clinical studies reveal stark inequality between how men and women’s bodies handle infections. Women have evolved to be particularly robust – fast and strong immune responses, likely to protect them during pregnancy and the postpartum period. (This immune protection, however, comes at a cost – women are also more likely than men to develop autoimmune diseases). Estradiol equips the body with potent protective anti-inflammatory effects, which could certainly come in handy during the “cytokine storm” resulting from the SARS-CoV-2 infection (Fig. 1) [11]. Estrogen-responsive immune parameters are going to be especially important during hormonal transition times like menopause when estradiol levels decrease and the body loses its protective effects, now being exposed to a ravaging onslaught of inflammatory processes [12].
Cortisol tends to get a bad rap, receiving the blame for anxiety, weight gain, insomnia, high blood pressure, you name it. It does all these bad things, but only when chronically high and not following a normal circadian rhythm. But we often forget that our bodies need cortisol to survive and having just enough cortisol around at the right time of day optimizes and boosts immunity while limiting inflammation [13, 14]. When stress doesn’t abate, however, too much cortisol can become destructive, opening the door for chronic immunosuppression. We are witnessing the COVID-19 pandemic unfold on a global scale, so it’s not surprising that all of us are affected and experience “empathetic stress” as we watch so many other people out there in distress and our own anxiety over the uncertainty of the situation. Keeping stress levels and, with that, normal circadian cortisol levels throughout the day, in check is going to be very important to maintaining a healthy immune response [15].
Vitamin D – typically called a “vitamin”, vitamin D is a precursor to a fat-soluble hormone – a substance that our skin produces in response to being out in sunlight. Vitamin D is best known to keep our bones healthy and strong by helping to assimilate calcium from our diet into skeletal tissues. At the gene level, the active form of vitamin D regulates the expression of hundreds of genes. Research shows that vitamin D is protective against acute respiratory infections [16].
Minerals like Zinc and Selenium – zinc can inhibit viral replication and shorten the duration of a common cold caused by a virus [17]; while selenium, forming part of selenoproteins including the antioxidant glutathione, contributes to our biggest defense system against the reactive oxygen species that viruses generate and contribute to the destructive inflammatory conditions in the lungs and heart at the late stages of COVID-19 infection.
As we wait for vaccine development against and testing for SARS-CoV-2 to ramp up, taking care of your health, starting with a healthy immune system, is going to be very important. Currently many doctors are transitioning from in-person appointments to telemedicine visits which presents an inherent problem in obtaining objective information like physical exams and labs. ZRT Laboratory is here to help by providing simple, minimally invasive lab testing from samples that patients can collect from the comfort (and necessity) of their own home.
Testing for Estradiol
Testing for Cortisol
Testing for Vitamin D
Testing for Elements
References
- Prompetchara, E., C. Ketloy, and T. Palaga, Immune responses in COVID-19 and potential vaccines: Lessons learned from SARS and MERS epidemic. Asian Pac J Allergy Immunol, 2020. 38(1): p. 1-9.
- Li, X., et al., Molecular immune pathogenesis and diagnosis of COVID-19. Journal of Pharmaceutical Analysis, 2020.
- Li, G., et al., Coronavirus infections and immune responses. J Med Virol, 2020. 92(4): p. 424-432.
- Chan, J.F., et al., A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet, 2020. 395(10223): p. 514-523.
- Zhao, Y., et al., Single-cell RNA expression profiling of ACE2, the putative receptor of Wuhan 2019-nCov. bioRxiv, 2020: p. 2020.01.26.919985.
- Thevarajan, I., et al., Breadth of concomitant immune responses prior to patient recovery: a case report of non-severe COVID-19. Nature Medicine, 2020.
- Huang, C., et al., Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet, 2020. 395(10223): p. 497-506.
- Wu, Z. and J.M. McGoogan, Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72314 Cases From the Chinese Center for Disease Control and Prevention. JAMA, 2020.
- Bouman, A., M.J. Heineman, and M.M. Faas, Sex hormones and the immune response in humans. Hum Reprod Update, 2005. 11(4): p. 411-23.
- Moulton, V.R., Sex Hormones in Acquired Immunity and Autoimmune Disease. Front Immunol, 2018. 9: p. 2279.
- Khan, D. and S. Ansar Ahmed, The Immune System Is a Natural Target for Estrogen Action: Opposing Effects of Estrogen in Two Prototypical Autoimmune Diseases. Front Immunol, 2015. 6: p. 635.
- Ghosh, M., M. Rodriguez-Garcia, and C.R. Wira, The immune system in menopause: pros and cons of hormone therapy. J Steroid Biochem Mol Biol, 2014. 142: p. 171-5.
- Venneri, M.A., et al., Circadian Rhythm of Glucocorticoid Administration Entrains Clock Genes in Immune Cells: A DREAM Trial Ancillary Study. J Clin Endocrinol Metab, 2018. 103(8): p. 2998-3009.
- Bahrami-Nejad, Z., et al., A Transcriptional Circuit Filters Oscillating Circadian Hormonal Inputs to Regulate Fat Cell Differentiation. Cell Metab, 2018. 27(4): p. 854-868 e8.
- Gamble, K.L., et al., Circadian clock control of endocrine factors. Nat. Rev. Endocrinol, 8/2014. 10(8): p. 466-475.
- Martineau, A.R., et al., Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ, 2017. 356: p. i6583.
- Science, M., et al., Zinc for the treatment of the common cold: a systematic review and meta-analysis of randomized controlled trials. CMAJ, 2012. 184(10): p. E551-61.
